By Michael Pottash MD MPH
Medical aid in dying (MAiD) is available to over 20% of Americans and is poised to become available to many more in the coming legislative cycle. In May 2023, my research team surveyed the American Clinicians Academy on Medical Aid in Dying. The Academy was organized as a non-membership organization to support clinicians caring for patients considering or completing MAiD. We aimed to investigate the practice and experience of clinicians who have been involved in MAiD work.
In the wider medical culture, the conversation about MAiD often centers on the ethical arguments about whether it ought to be a part of medical practice. Below I wish to highlight several points from our findings that suggest efforts to improve the provision of MAiD may be just as important.
In a very rough approximation, 64 clinicians wrote nearly a third of all prescriptions in the country.
I have heard health system administrators ask whether MAiD is best provided by a few specialized clinicians or by the many clinicians who care for patients suffering with a serious illness. Should policies be written to emphasize a deep understanding and knowledge of MAiD or should they be written to emphasize longitudinal relationships? The tradeoff here is that specialized clinicians may not know the patients as intimately but will have a deeper knowledge of MAiD practice and bureaucratic hurdles.
In our survey we invited respondents to provide an estimate of how many MAiD prescriptions they had written. When our survey respondents reported some very large numbers, I got curious about how our data compared with the publicly available state data. What proportion of the 13,808 publicly reported MAiD prescriptions written since Oregon began collecting data in 1998 can be ascribed to our survey respondents?
States report the number of clinicians writing prescriptions each year, but they don’t provide information on how many are repeat prescribers or how many prescriptions each prescriber writes. They do report prescriptions by year and so this allowed me to compare our numbers with state data. For purposes of analysis, when a respondent provided a range, we took the average of that range; or when a clinician had written “>100,” this was counted as 100. Another caveat: Our data includes the beginning of 2023 while in most cases, the data from the states only includes prescriptions through 2022. With that in mind, here is how the data breaks down by state:
| State | Prescriptions written through 2022 | Prescriptions written by survey respondents through May 2023 | Number of survey respondents per state | Percent of prescriptions written by survey respondents |
| California | 5,168 | 2,269 | 30 | 44% |
| Colorado | 1,090 | 508 | 8 | 47% |
| District of Columbia | 31* | 25 | 1 | 80% |
| Hawaii | 197 | 115 | 2 | 58% |
| Maine | 172 | 75 | 1 | 44% |
| New Jersey | 186 | 109 | 4 | 59% |
| New Mexico | No reporting | 127 | 8 | n/a |
| Oregon | 3,712 | 885 | 7 | 24% |
| Vermont | 115** | 50 | 2 | 43% |
| Washington | 3,137 | 337 | 7 | 11% |
| Total | 13,808 | 4,544*** | 64 | 33% |
**Through June 2021
***Includes two respondents who prescribe in multiple jurisdictions but excludes New Mexico.
My very rough state by state calculations reveals that in many states, a small number of clinicians are doing a large quantity of the MAiD prescribing. Leaving out New Mexico (where there is no publicly available data) 64 clinicians responding to our survey reported an estimated 4,544 MAiD prescriptions through May 2023. While these are some back-of-the-napkin calculations, they suggest that somewhere around a third of all MAiD prescriptions have been written by a comparatively small number of clinicians.
25% of responding clinicians trained in hospice and palliative medicine.
My bias as a palliative care clinician and educator is to prefer that terminally ill patients (especially those considering a palliative option of last resort) be cared for by clinicians with palliative care specialty training, or at least in the setting of a hospice or palliative care practice. Requests for hastened death are complex and how we interpret, explore, and answer such requests will vary depending on training and clinical culture. I’ll admit that it makes me nervous that only 25% of respondents trained in hospice and palliative medicine and only 33% describe their practice as hospice or palliative care. Meanwhile 22% of clinicians described their practice as a specialized “aid-in-dying practice.”
However, clinicians of many backgrounds have always been involved in the care of those with serious and terminal illnesses. Hospice and palliative care clinicians are divided about whether they ought to engage with MAiD. Furthermore, many hospices have religious affiliations that inform prohibitive policies toward MAiD. Engaging a clinician with experience and specialization may be the most prudent, especially since legacy healthcare societies are not providing guidance or counsel.
Clinicians feel that they should “sometimes” raise the option of MAiD with patients.
One of the responsibilities of informed consent is to provide patients with alternatives when discussing a given treatment plan. It’s an axiom of medicine that if an option hasn’t been raised with a patient, we can’t assume that we have discharged our clinical responsibility to inform. This creates a very sticky paradox when it comes to MAiD.
In our survey we asked clinicians: How often do you introduce the option of MAiD with eligible patients who have not raised it themselves?
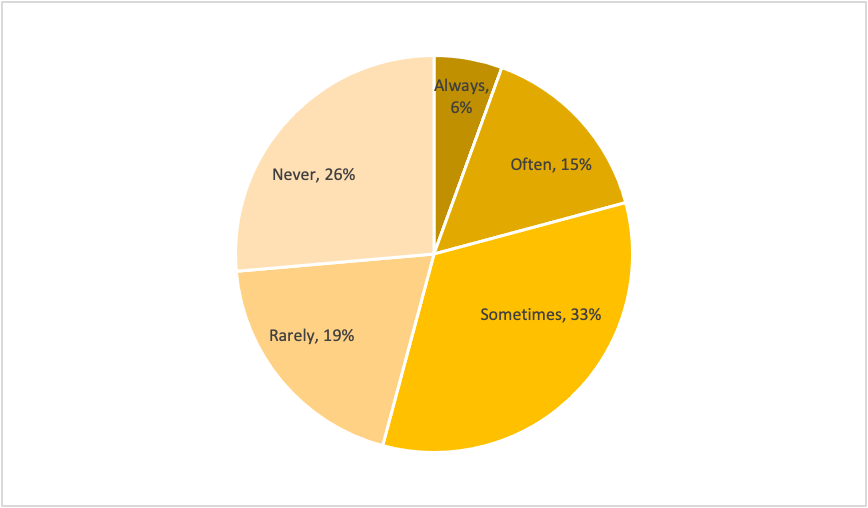
As you can see in the figure, there was no consistent practice, even among this experienced cohort. The average answer to this question was “sometimes.” And this was true even among clinicians who describe their practice as a specialized “aid-in-dying practice” and who mostly care for patients who come to their clinic for MAiD!
One could argue that terminally ill patients may not know that they live in a jurisdiction where MAiD is legal if clinicians do not inform them of this fact. There may even be an equity corollary where better informed, more resourced patients are more likely to know about MAiD and an effort to improve access for less informed patients is to conceptualize an affirmative duty to inform. On the other hand, clinicians feel very uncomfortable with raising the option of MAiD with their terminally ill patients. No clinician wants to be perceived as encouraging a terminally ill patient to hasten their death.
The big picture
There are two parallel conversations happening in this country: one is about whether MAiD should be an option at all and the other is how to do it well. Our survey findings remind me that there are many consequential questions still to be answered: Should patients seeking MAiD be referred to specialized clinicians? What training prepares a clinician to best care for seriously ill patients seeking MAiD? In what setting should these patients be cared for? How do we make sure that patients understand all of their end-of-life options?
The big ethical, moral, and philosophical questions raised by MAiD are fascinating and yet, the polls suggest that MAiD is popular enough to continue expanding. I wonder if the clinicians who are deeply involved in the care of the terminally ill and think of themselves as against the practice of MAiD might better serve their patients by turning their focus towards improving the practice of MAiD rather than arguing that it has no place in medicine.
Michael Pottash MD MPH is a palliative medicine physician at MedStar Washington Hospital Center and associate professor of medicine at Georgetown University School of Medicine.


One thought on “Medical Aid in Dying’s Other Conversation”
Comments are closed.